The envelopes have been opened. Fates – at least for the next 3-7 years – have been determined. Tears – hopefully of joy – have been shed. And just like that, another Match Day is in the books.
And you know what that means.
Yup, that’s right.
It’s time to break it down, Winners & Losers™️ style.
–
–
LOSER: Emergency medicine programs.
The big story in the 2023 Match has been the number of unfilled positions in emergency medicine (EM). Only 82% of EM positions filled, which was the lowest of all major specialties with the exception of radiation oncology (81%).
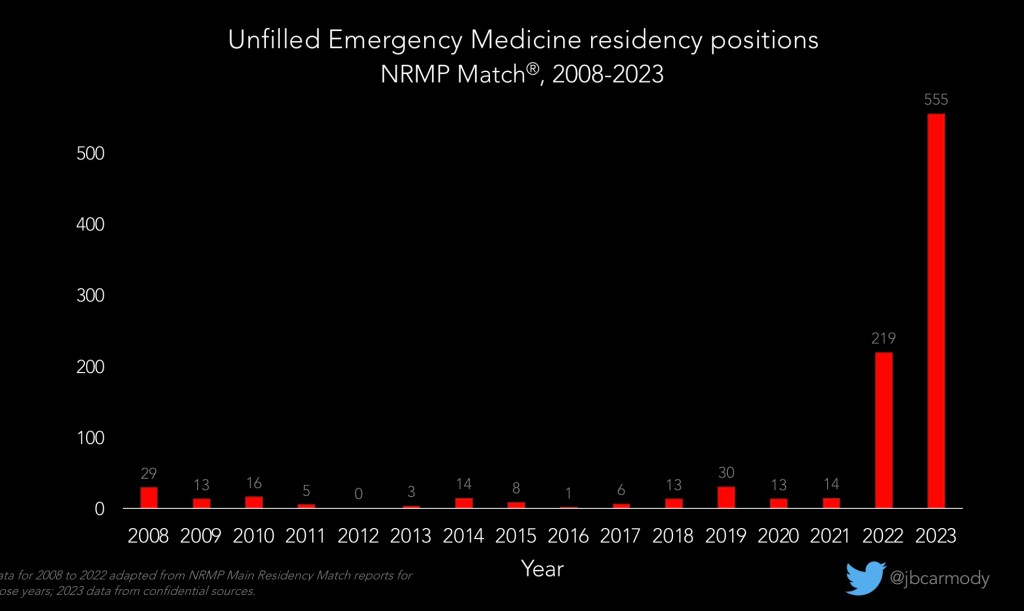
Of course, this is only a surprise if you haven’t been paying attention – I predicted it in the fall after the ERAS preliminary data came out. But that hasn’t kept certain media outlets from covering this like it’s a moral panic.
Look, there’s definitely a conversation to be had about the future of EM. But as we have that conversation, let’s remember that the number of unfilled positions is an imperfect surrogate for anything we really care about.
In fact, lemme give you a bold prediction for next year: the number of unfilled EM positions will decrease in the 2024 Match- even though the number of applicants from U.S. medical schools will continue to decline.
Why? EM programs will adjust their recruiting strategies, and international medical graduate (IMG) applicants will respond to the changing landscape by applying to EM in greater numbers. In other words, the number of unfilled positions will decrease without any fundamental difference in the experience of being an emergency medicine physician.
(Heck, while I’m at it, I’ll give you another bold prediction for next year: the “SOAP crisis” infecting EM will spread to pediatrics in 2024. The number of applicants to pediatric residency programs has been in decline, even as the number of programs expands – and many program directors aren’t yet paying attention. My guess is we’ll reach a tipping point next year and the number of unfilled pediatric positions will be >200. Just remember, you heard it here first.)
–
WINNER: Diagnostic radiology.
Many emergency medicine program directors want to know: where did their applicants go? Based on nothing more than the application and match data, the likely answer seems to be diagnostic radiology.
This year, every single one of the 1176 diagnostic radiology positions offered in the Match filled. (The only other specialties to fill 100% of their positions were orthopedic, plastic, and thoracic surgery.)
–

LOSER: Family medicine.
It was another lean year for many family medicine programs.
Only 88.7% of family medicine positions filled, leaving 577 left over (23 more than the number of available EM positions).
Just 29% of the available family medicine positions were filled by graduating U.S. MD students, with another 30% filled by graduating DO students – meaning that U.S. medical schools only produce enough students to fill a little more than half of the family medicine positions offered.
–
WINNER: Match data misinterpretation.
It happens every year.
Within minutes of the release of the NRMP’s Advance Data Tables, I start to hear chatter on social media discussing shockingly low specialty match rates.
This year, for instance, I’ve heard folks claim that the 2023 Match had a 69% match rate for graduating MD students entering anesthesiology, and a 72% match rate for the same group entering general surgery.
Sigh.
The problem is that the NRMP’s Advance Data Tables and Main Match reports can’t distinguish applicants who really want to match in that specialty from applicants who are applying as a backup.
So it’s true that 1741 MD seniors applied to PGY-1 positions in anesthesiology. And it’s true that only 1199 of them matched. And it’s also true that 1199/1741 = 69%.
But what’s entirely unknown is how many of the applicants who didn’t match in anesthesiology actually into a more preferred specialty (and applied to anesthesiology programs as a backup).
To get the real match rates, we need to know an applicant’s preferred specialty – and only the NRMP’s Charting Outcomes in the Match reports tell us that. (If you’re interested, you can peruse match rates for graduating MD students, graduating DO students, and international medical graduates for the 2022 Match.)
(That said, few applicants are bold enough to apply to uber-competitive specialties like orthopedics, plastic surgery, or otolaryngology as backups – so the respective 73%, 75%, and 82% match rates you’d estimate from the advance data are likely to be very close to reality.)
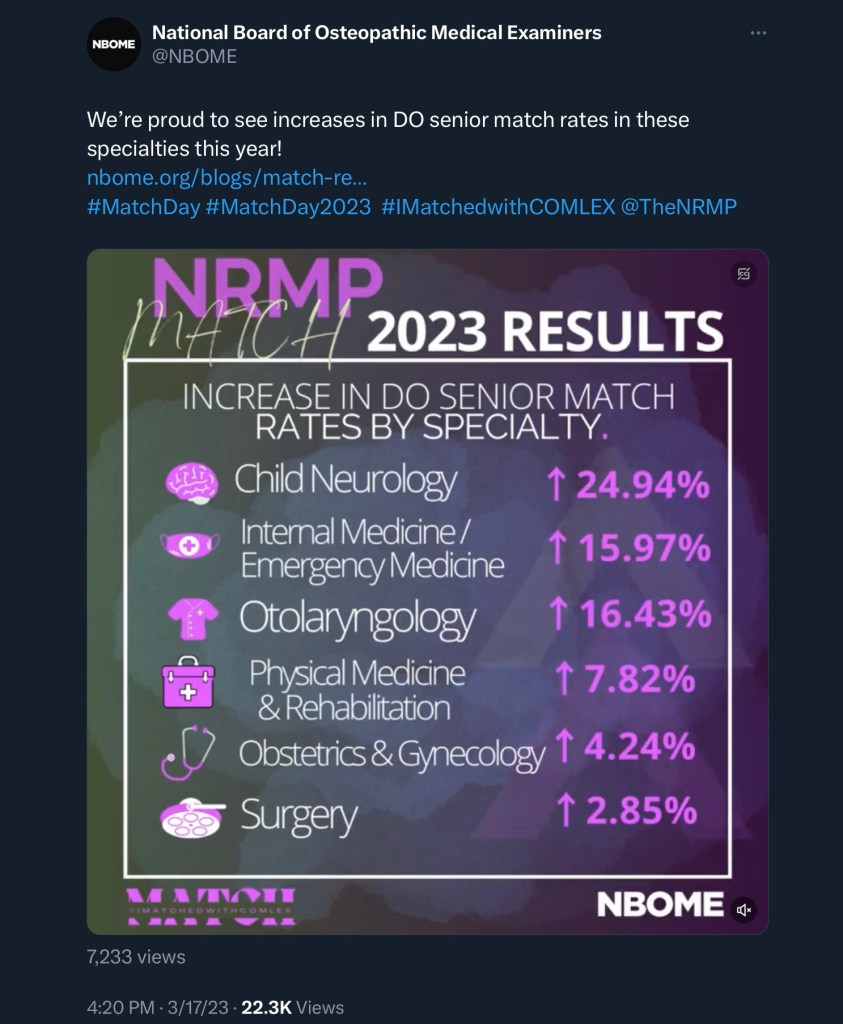
Other variations of misinterpretation are even more bizarre. On Twitter, the National Board of Osteopathic Medical Examiners celebrated improvements in DO senior match rates… and I truly have no clue how they calculated their figures. (Naturally, though, they declined to provide any explanation.)
–
WINNER: Match rates.
Even though we don’t know specialty-specific match rates, we do know the overall match rate – which, at 81.1% for all applicants submitting a rank order list, was the highest in the modern era.
Actually, the match rate for graduating DO students and U.S. citizen international medical graduates hit all-time highs at 91.6% and 67.6%, respectively. Meanwhile, 93.7% of graduating U.S. MD students matched, which is up slightly from last year, and counts as the highest match rate since the COVID-19 pandemic.
–
LOSER: Non-U.S. citizen IMGs.
Not all applicant groups saw record-setting match rates, however. Non-U.S. citizen IMGs matched at a 59.4% rate, up only slightly from last year’s 58.1%.
Why did U.S. citizen IMGs fare so much better than their non-U.S. citizen counterparts this year? The answer is likely related to the specialties that these groups tend to target.
While both U.S. citizen and non-U.S. citizen IMGs most commonly match into positions in internal medicine or family medicine, relatively more U.S. citizen IMGs target positions in emergency medicine and psychiatry – specialties that were less competitive this year than in recent application cycles. Conversely, more non-U.S. citizen IMGs apply in neurology and pathology, specialties that proved to be surprisingly competitive (with program fill rates of >99% for each).
–
LOSER: Couples.
Another group that didn’t fare as well in 2023 was couples, who had a match rate was 93% – down from the >95% rates recorded between 2016 and 2020.
Ninety-three percent doesn’t sound too bad… but here, it’s important to note that many couples submit rank order lists in which one partner goes unmatched. Yet because the matching algorithm assigned a pairing that they said they were willing to take, this gets recorded as a successful match.
In fact, only 88.4% of couples received a pairing in which both partners received a residency placement.
–
WINNER: Match rate fibs.
Now that Match Day is over, we can all look forward to a series of self-congratulatory press releases from medical schools, claiming match rates of 98-100% for their students. (For instance, every DO-granting medical school but one claims a match rate that’s higher than the national average match rate for DOs.)
In reality, most medical schools conflate their match rate (the proportion of students who are assigned a residency position in the Match) with their placement rate (which includes students who went unmatched but managed to get an unfilled position after the Match was over).
From the schools’ standpoint, this distinction may not matter – their students got a residency position, right? But for a student who missed the chance to train in their dream specialty and instead had to settle for a one-year preliminary position and the uncertainty of trying to match again in a year, it’s a big deal.

For pre-meds considering these advertised match rates when making their school selection, all I can say is caveat emptor.
–
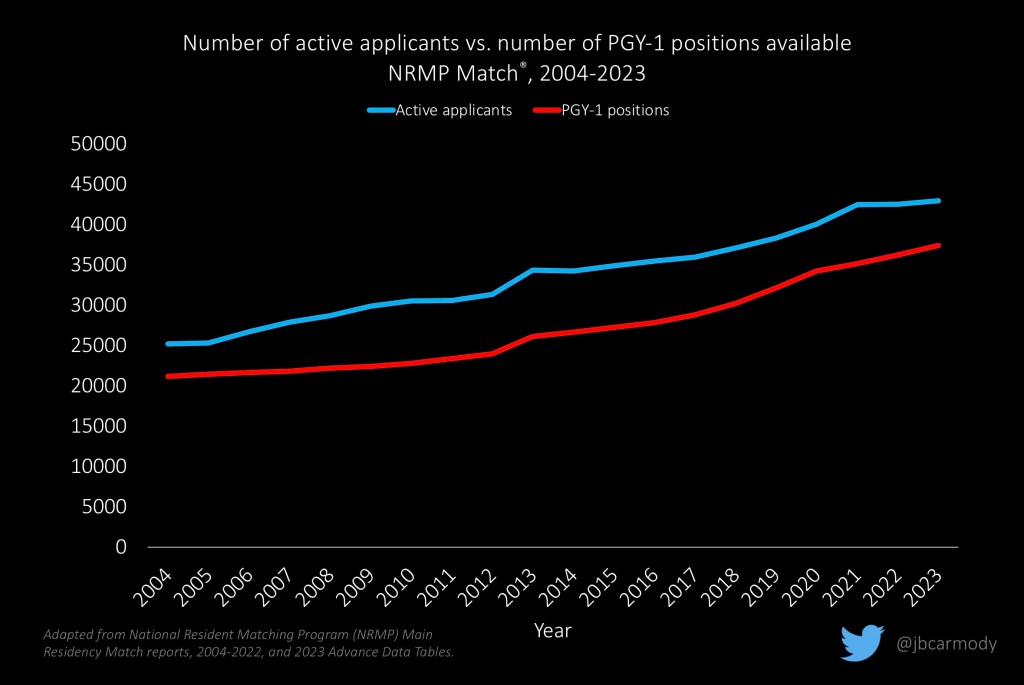
LOSER: The “residency positions aren’t growing!” reply guys.
For as long as I’ve been talking about things in this space, I’ve followed with curiosity a vocal and diverse group who claim – despite evidence to the contrary – that the number of residency positions isn’t growing, or at least that it’s not growing at the same rate as medical graduates.

But don’t worry, Lil’ Cartoon Doctor Dude, it’s not true!
It’s true, if you take all comers, there are more residency applicants than there are residency positions. But there’s no evidence that disparity is widening – and in fact, this year’s NRMP data suggest it’s closed a bit.
–
LOSER: The unmatched.
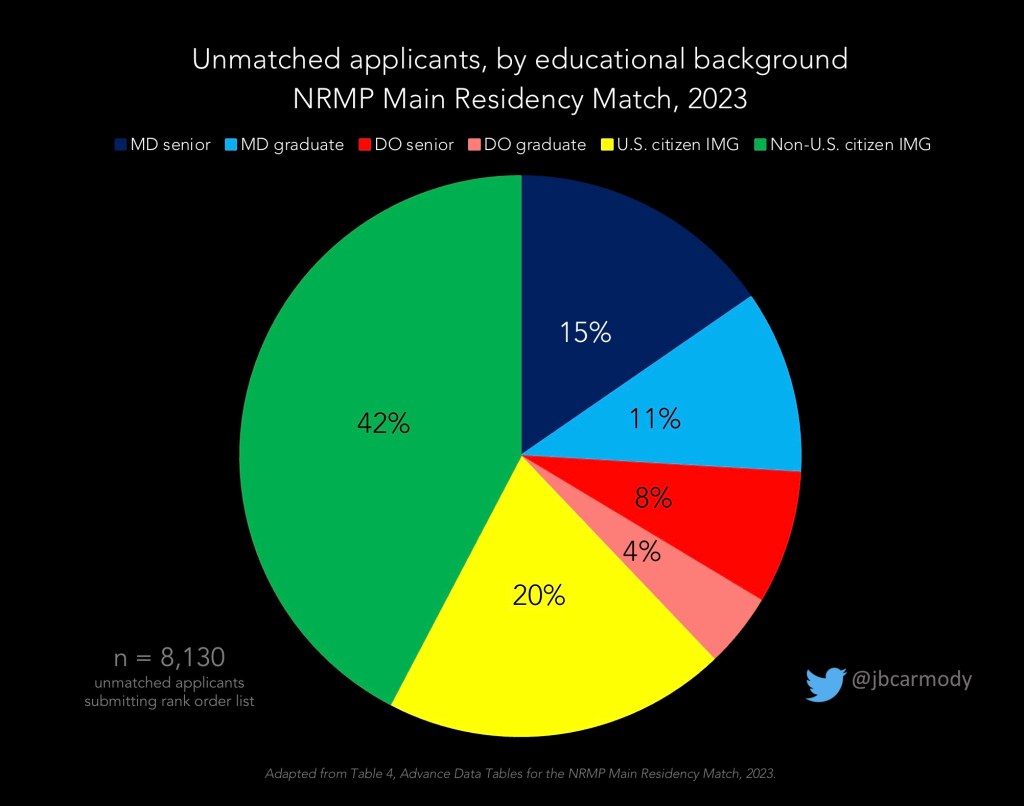
Even with a record-setting overall match rate and growth in the number of residency positions, there were still a lot of applicants who went home empty-handed on Match Day: 8,130 applicants who submitted a rank order list did not match to any PGY-1 position. Another 3,049 never submitted a rank order list (likely because they received no interview offers), but stuck around for the SOAP.
–
LOSER: USMLE Step 1 apologists.
This year was the first year that many residency applicants applied without a USMLE Step 1 score.
Before the test moved to pass/fail scoring in January 2022, we heard dire warnings from the Step 1 apologists questioning how selective specialties could possibly choose their applicants without a three-digit measure of basic science knowledge to guide them. And yet, somehow, some way, competitive residency programs managed to find applicants and fill their programs.
–
WINNER: The Electronic Residency Application Service (ERAS).
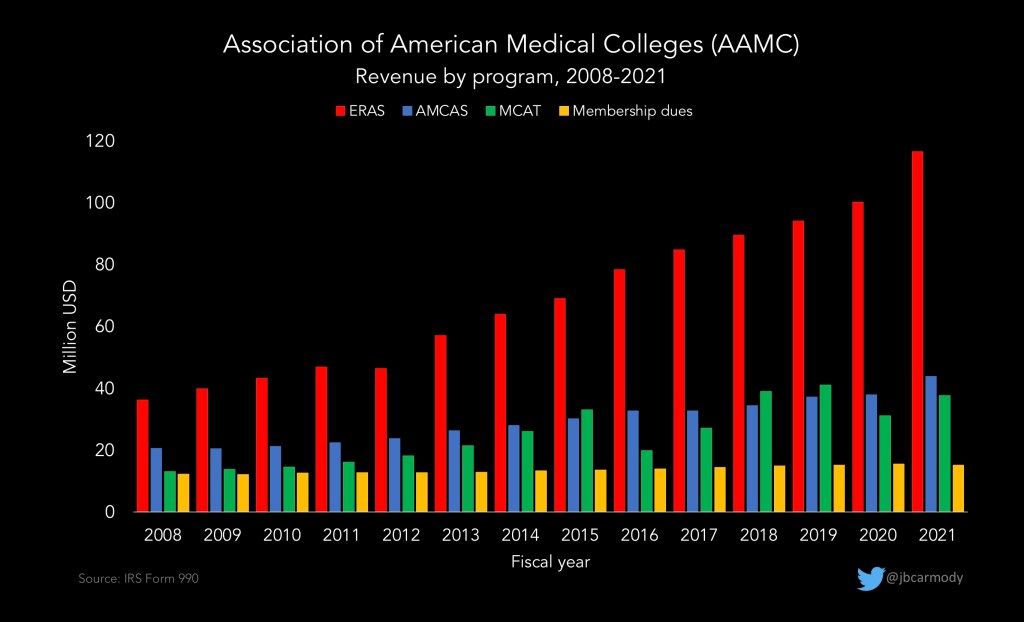
Unlike previous years, ERAS managed to make it through SOAP week without crashing and suffering prolonged downtime. Maybe some of the skyrocketing revenue from residency applications is being put to good use.
–
WINNER: Preference signaling.
Although certain specialties – like otolaryngology – have used preference signaling for several years, the 2022-2023 season marked the first year that almost all specialties allowed applicants to send a limited number of signals to their favorite programs before their application was reviewed.
Anecdotally, the expansion of preference signaling seems to have gone well. I’m sure numerous papers are forthcoming describing signaling in the new specialties – but for now, the best data come from the otolaryngology experience, which has been favorable. In this highly-competitive specialty, at least, signaling seems to lead to a better distribution of interview offers (slightly fewer for the top applicants, but more for everyone else), and doesn’t disadvantage women or minority groups.
–
LOSER: Preference signaling gamers.
Although many applicants don’t realize it, on Match Day, program directors (PDs) receive a report listing where all of their ranked applicants ultimately matched.
(So yeah, if you sent a love note saying you were ranking a program number one, but didn’t – the program will know, and will see who you ranked over them. You may want to avoid that program for your fellowship applications.)
But this year, some PDs have been surprised to see some of their preferred applicants matching not just at other programs – but in other specialties altogether, even though those applicants sent a signal of interest.
The issue is that in the rat race of residency selection, some applicants have realized they could gain advantage by applying to multiple specialties – and utilizing the preference signaling system of each. Consider an applicant who dreams of becoming a surgeon. She applies to 100 general surgery programs, and signals 5 of them. But then, to ensure she matches, she also applies to 5 anesthesiology programs – and sends signals to each of them, too.
The anesthesiology programs are likely to give her an interview – and based on the signal sent with the application, would have reasoned that their program was in her top 5. But in reality, it wasn’t even in her top hundred.
As more PDs puzzle over their match results, they’re likely to call upon ERAS to eliminate this opportunity to game the system by requiring applicants in future cycles to select a preferred specialty – and limit preference signaling to that specialty only.
–
WINNER: Non-first choice matchers.
For some applicants, the joy of Match Day was tempered by opening their envelope and seeing a placement that wasn’t what they’d hoped for.
It can feel like a gut punch. So it may help to know that you’re not alone: even though overall match rates remain high, there’s been a slow and steady decline in the proportion of graduating MD students who get their first choice.
It may also help to know that, ultimately, it may not matter.
If you survey medical students right after Match Day, the happiest and most satisfied ones are those who matched higher on their rank order list. But ask them again 3 months into intern year, and everyone is indistinguishable.
Ultimately, your residency and career are what you make of them – and to everyone who survived Match Day 2023, I wish you my very best.
–
YOU MIGHT ALSO LIKE:
Match Day 2021: Winners & Losers Edition
Match Day 2022: Winners & Losers Edition